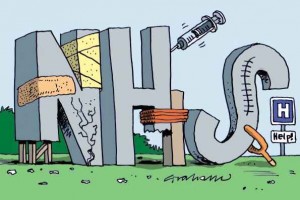
High street health the key to NHS survival
 It may be a heatwave outside but the College of Emergency Medicine focused our attention on colder days ahead with a warning that the NHS faces ‘walking blindfolded into another ‘winter crisis’’ if it doesn’t take action, and helpfully provided its solutions. All very reassuring until I scanned the 13 practical recommendations put forward by clinicians working in busy A&E units and realised there was no mention of community pharmacy – no suggestion that not only did many of these people not need to be in A&E, they probably didn’t need to see a GP either.
It may be a heatwave outside but the College of Emergency Medicine focused our attention on colder days ahead with a warning that the NHS faces ‘walking blindfolded into another ‘winter crisis’’ if it doesn’t take action, and helpfully provided its solutions. All very reassuring until I scanned the 13 practical recommendations put forward by clinicians working in busy A&E units and realised there was no mention of community pharmacy – no suggestion that not only did many of these people not need to be in A&E, they probably didn’t need to see a GP either.
A&E attendances continue to rise as people cannot get GP appointments, or regard emergency departments as the ‘go-to’ for all health complaints, big or small as they are likely to be seen in a few hours. GP attendances are also rising, due in part to the increasing number of patients with long-term conditions, yet common ailments such as coughs and colds, account for a fifth of a GP’s workload – over 50 million consultations every year. It shouldn’t take a genius to work out that if people were encouraged to go to their community pharmacist or other high street health professionals like optometrists or dentists, for common conditions, GPs would have greater capacity to manage patients with more complex needs, and hopefully have more appointments available so that people didn’t go straight to A&E when they can’t get a timely appointment. Convenient locations and extended opening hours means that high street health specialists are an appropriate alternative to GPs and A&E for thousands of patients.
A solution for an acute problem, but a report published this week, ‘We Are Primary Care’, makes it clear that if we want to reduce pressures on A&E and GPs in the longer term, we need to start thinking in terms of prevention rather than cure, tackling life-style related conditions that are using an ever-increasing share of limited NHS resources. Long-term conditions cost £7 in every £10 spent on health and social care in England and the number is set to rise by at least 25% over the next 15 years. Eating badly, smoking and drinking combined with less exercise are all factors driving a huge increase in the prevalence of diabetes and other long term conditions, with huge financial implications for limited NHS resources.
With over 1.2 million people visiting over 11,500 community pharmacies in England every day for health-related reasons, there are nearly half a billion opportunities yearly to talk to people about their health and wellbeing and move from ‘sick-care’ to ‘self-care’. If NHS services are to remain accessible and available to everyone who needs them, we need to look beyond A&E and GPs as the only access points for the NHS and start treating ourselves better with the help of our health specialists on the high street..

